What is Lung Fibrosis?
COVID-19 is certainly leaving its mark on the world. The virus has infected nearly 150 million people worldwide. Those infected note a range of symptoms from fever, dry cough and tiredness to difficulty breathing, pneumonia, acute lung injury (ALI), acute respiratory distress syndrome (ARDS) and lung fibrosis.
COVID-19 attacks the respiratory system. It binds to the surface of the lung epithelium: the cells lining the airways. When this happens, our immune system responds, and immune cells are activated in an attempt to contain the infection, stopping it from spreading and destroying the virus. Our immune cells, namely macrophages and dendritic cells, stimulate the production of cytokines (signalling molecules) which activate more immune cells, such as natural killer cells (NK cells) and T helper cells. More cytokines (a cytokine storm) are released to activate NK cells further.
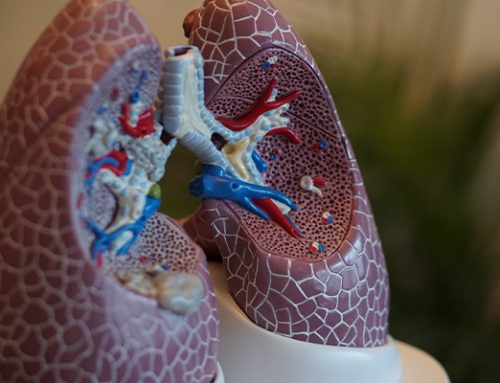
NK cells, macrophages and neutrophils release compounds such as reactive oxygen species (ROS) and nitric oxide (NO) intended to destroy the virus and infected or damaged cells. However, these compounds can also damage the lung epithelium. In response to the damage, macrophages and other cells deposit collagen to structurally support the damaged area in a process called tissue remodelling. In some cases, the collagen can be deposited right throughout the lungs, and the thick, fibrous collagen material creates scarring, making the lung tissue inflexible. This is known as lung fibrosis.
The infiltration of immune cells leads to swelling, which can also contribute to lung inflexibility and thickening of the alveoli walls. Damage to the epithelium allows fluid to accumulate in the alveolar spaces leading to further swelling. COVID-19 also binds to ACE2 (angiotensin-converting enzyme 2) receptors in the lungs. ACE2 is thought to regulate lung oedema (swelling), and inhibition of ACE2 by COVID-19 increases lung oedema.
An increasing number of COVID-19 survivors continue to battle symptoms long after they test negative for the disease. This has been termed “long COVID”. As with the viral infection itself, long COVID symptoms can vary from mild, such as fatigue or body aches, to severe, including cardiac abnormalities and lung fibrosis. Various studies indicate that around 70-80% of COVID-19 survivors have at least 1 symptom that persists even after they test negative for the virus. Further, it is estimated that around one-third of patients hospitalised with COVID-19 develop lung fibrosis. Development of fibrosis is linked to the length of time a patient has COVID-19, with 61% of patients who had the disease for longer than 3 weeks developing fibrosis, compared to only 4% who were infected for less than a week.
In one case report on post-COVID lung fibrosis, a 60-year-old man presented to the hospital with a persistent dry cough. Four months earlier, he had been treated for moderate COVID-19 pneumonia. After successful treatment for pneumonia and being asymptomatic for 10 days, he was discharged. He remained symptom-free for around one month but then developed a dry cough that worsened over time. Upon re-admission, he was found to have lung fibrosis. This case shows that even with timely and adequate treatment of COVID-19 infection, fibrosis can still develop later.
There are several risk factors for developing lung fibrosis from COVID-19, including age, comorbidities (having other diseases such as hypertension, diabetes and cardiovascular disease), prolonged hospital admission, particularly with mechanical ventilation, smoking and possibly excessive alcohol intake.
Lung fibrosis is a progressive disease with no known medical cure. People with lung fibrosis often present with shortness of breath, a persistent, dry cough, fatigue, weight loss, body aches and clubbing – the widening of the tips of the fingers or toes. Unfortunately, the scarring in lung fibrosis is thought to be permanent once it has developed, although its progression can be slowed by medications, such as corticosteroids, anti-inflammatory agents and anti-scarring agents. Oxygen supplementation may also be prescribed to help make breathing and exercise easier, improve sleep and increase blood oxygen levels. In severe cases, a lung transplant may be required to improve quality of life and extend life.
Dietary modifications and supplementation are increasingly important as patients with chronic pulmonary conditions seek non-invasive and non-pharmaceutical ways to support treatment and prevent disease progression. Several classes of bioactive compounds, such as anthocyanins, found in fruits have potent anti-inflammatory properties that may target the inflammatory cytokines that become dysregulated during lung remodelling, helping to switch these innate immune factors back into healing and recovery mode.
BerriQi® is a patented Boysenberry and apple ingredient scientifically proven to reduce mucus production, resolve lung inflammation and repair chronic inflammatory damage (fibrosis).
A natural whole fruit solution, boysenberry anthocyanins and ellagitannins plus apple procyanidins have been shown to contribute to various molecular pathways and cellular mechanisms related to the resolution of inflammation and post-inflammatory repair of airway tissue. Backed by science, BerriQi may offer much-needed health benefits for consumers suffering from lung fibrosis.
Support groups for those living with lung fibrosis (also known as pulmonary fibrosis) can be found online and in the community. These groups are a great option to learn about the disease and available treatments, navigating the medical system, and improved coping strategies and lifestyle modifications.