You know the feeling—when your throat starts to scratch and tickle, your temperature fluctuates, your skin gets sensitive… It’s the start of an illness.
There’s a brief window when perhaps you try to nip it in the bud with immune support supplements, vitamin C, and a nap with your fingers crossed that it won’t progress into a full-blown respiratory infection. Sometimes your early efforts pay off and it amounts to nothing; other times, however, it takes days in bed to regain energy, and sometimes it’s a matter of weeks or even months before the runny nose and cough symptoms fully clear up.
So what is happening at each of these phases of a respiratory infection? More importantly, how can we support our immune systems at every phase?
Prevention
Most of the time, we aren’t aware we’re fighting viruses and bacteria entering our airways because our immune systems have developed specific antibodies that prevent an infection from taking hold. This adaptive immunity develops during prior exposures to a pathogen, either last season or by way of a vaccine which provides a recognisable part or a weakened version of the pathogen.
The next best way to prevent infections is by supporting our innate immune system which handles novel pathogens that our immune systems don’t recognise. We can support our innate and adaptive immunity by getting an average of 8 hours of sleep each night, getting regular exercise, eating a balanced diet with lots of colourful fruits and vegetables, and managing stress. Even if a pathogen slips through your defences, these habits will give you the best chance of beating an infection quickly and making a speedy recovery.
Panic!
Early symptoms of a cold or flu appear suddenly: fatigue and exhaustion set in, appetite disappears, muscles ache, skin tingles, throat scratches, sinuses fill up, and a fever and chills appear out of nowhere. This is your body’s immune system diverting as many resources as it can towards fighting a pathogen that is rapidly replicating in your respiratory tract.
At this point your innate immune system is running the show. A huge and complex cohort of innate immune cells, also known as effector cells, are at work and largely responsible for the symptoms we experience. Effector cells are phagocytic, meaning they engulf pathogens and dying cells, preventing the release of replicating pathogens. Many phagocytic cells are also granulocytes, which contain small granules of potent chemicals that kill pathogens.
The release of phagocytic cells from tissues, along with the increase in number of phagocytes circulating in the blood stream, and the release of and chemicals from granulocytes create the inflammatory response and are very effective at fighting viruses and bacteria. This is the time when immune stimulants like elderberry and manuka honey are helpful because they support the activity of the innate immune system.
Peak Yuck

At this point fevers are common. A fever, otherwise known as pyrexia or a febrile response, is part of this inflammatory response, although it’s controlled by an area of the brain called the hypothalamus. A fever is another way of creating a hostile environment for the invading pathogen, making it weaker and less able to reproduce. Unfortunately, it also creates a hostile environment for us to exist in as well. But those innate effector cells seem unbothered by the elevated temperature. In fact, they seem to thrive.
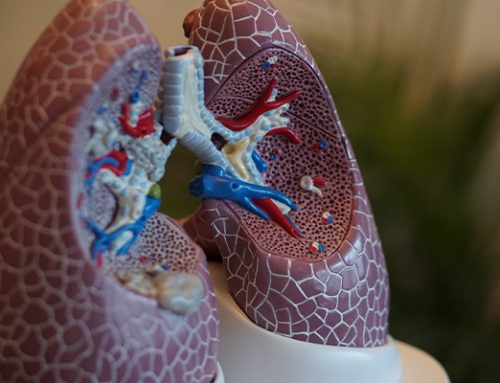
One type of effector cells of particular interest in the context of respiratory infections are tissue-resident cells called Macrophages. Specifically alveolar macrophages located in the tissue around the air sacks in the lungs are some of the first responders when a pathogen is detected. Alveolar macrophages are deployed in what’s called the M1 state.
M1 macrophages act like an aggressive yet compelling cavalry leader, recruiting more troops (eosinophils and neutrophils) to the battle site. This influx of phagocytic granulocytes waging chemical warfare in the delicate air sacks of the lungs can feel brutal, as the increased numbers cause swelling. Plus, a lot of local collateral damage occurs while the immune system destroys invaders.
To address this, M1 macrophages and some of their mates prompt the cells lining the lungs to produce supportive collagen, but that is only meant to be temporary. In a valiant attempt to clear the wreckage, lungs produce mucus to capture the remains of both the invading pathogen and our own sacrificial immune cells, to be carried out of the lungs through coughing… Probably at the most inconvenient and annoying times, like while trying to get some much-needed sleep.
This is the time when both immune stimulants and anti-microbial products like manuka honey are still helpful, but the addition of overall support, for instance zinc and vitamin C-rich lemon juice, is needed because the body has been working extra hard for several days. There’s also evidence that mitochondrial support such as CoQ10 can be helpful in the midst of a bout with the flu, as those immune responses are very demanding of the energy-supplying mitochondria within cells.
Sweet relief. Recovery

At some point, all things going well, the infection will have run its course, the fever will subside, and many of the aches and pains will ease, thanks to granulocytes now keeping their toxic contents to themselves.
Your body will still be trying to clear out the mess and rebuild damaged tissues, which can feel like general fatigue, an ongoing cough, and an itchy, irritated airway where repairs are taking place near nerve endings… like the itchiness that occurs as a scab turns into a scar and collagen is deposited over an abrasion.
While most immune cells have either done themselves in as kamikaze fighters or returned to their stations, there are some immune cells that don’t find it quite so easy to turn off after a fight. M1 macrophages can get stuck in this aggressive state even after an infection has been cleared, continuing to recruit other immune cells and cause symptoms, now continuing a futile cycle of collateral damage and collagen scaffolding after the pathogen has gone.
What’s needed to make a full recovery is for M1 macrophages to lay down their M1 swords, switch to janitor mode and pick up their M2 macrophage brooms, tell their mates to go home, and help clean up some of the structural supports they previously built to support the effort.
For instance, collagen support in the damaged areas becomes unhelpful and restrictive scar tissue where it’s preferable to have flexible tissue to allow the expansion and contraction of breathing. M2 macrophages switch on the tools to break that collagen down before it’s problematic. M2 macrophages also direct other immune cells back to their happy places, making more space for bigger breaths and reducing the feeling of irritation in the airways.
The transition from recovery to resolution can be the longest and most drawn-out phase of an illness, with symptoms lingering for days, weeks, or even months. At this point, immune balancing BerriQi comes to the rescue. BerriQi is scientifically proven to promote the switching of Macrophages from M1 to M2, significantly reduce the number of immune cells in the lungs, reduce mucus production, and reduce collagen in the interstitial space.
Resolution. Finally.
References
BUHARFEIL, N; AL ORAN, L; ABO-SHEHADA, M (2008) The effects of bee honey on the proliferative activity of human B and T lymphocytes and activity of phagocytes. Food and Agricultural Immunology (11): 169- 177
CHARYASRIWONG, S; HARUYAMA, T; KOBAYASHI, N (2016) In vitro evaluation of the antiviral activity of methylglyoxal against influenza B virus infection. Drug Discoveries & Therapeutics, 10: 201-210.
Chase, M., Cocchi, M. N., Liu, X., Andersen, L. W., Holmberg, M. J., & Donnino, M. W. (2019). Coenzyme Q10 in acute influenza. Influenza and other respiratory viruses, 13(1), 64–70. https://doi.org/10.1111/irv.12608
Shaw, O. M., Hurst, R. D., Cooney, J., Sawyer, G. M., Dinnan, H., & Martell, S. (2021). Boysenberry and apple juice concentrate reduced acute lung inflammation and increased M2 macrophage‐associated cytokines in an acute mouse model of allergic airways disease. Food science & nutrition, 9(3), 1491-1503.
Shaw, O. M., Hurst, R. D., & Harper, J. L. (2016). Boysenberry ingestion supports fibrolytic macrophages with the capacity to ameliorate chronic lung remodeling. American Journal of Physiology-Lung Cellular and Molecular Physiology, 311(3), L628-L638.
Watanabe, K; Rahmasari, R; Matsunaga, A; Haruyama, T; Kobayashi, n (2014) Anti-influenza Viral Effects of Honey In Vitro: Potent High Activity of Manuka Honey. Archives of Medical Research 45 (5): 359-365.