In the simplest terms, inflammation is our bodies’ immune system’s response to pathogens, damaged cells or irritants such as pollution. Acute inflammation is the initial response, involving activation of the system, destruction of the offending stimuli, healing of any damage sustained during this process, and then ceasing. Chronic inflammation is a long term ongoing simultaneous damaging and healing process, frequently without resolution.
Inflammation is a normal response to harmful stimuli. It is part of our bodies’ innate immunity, in contrast to adaptive immunity, which is specific to particular invaders. Too little inflammation and the site of stimulation may be damaged by the invading stimuli, particularly if it is harmful such as a pathogen, potentially compromising survival. Too much and chronic inflammation may result, or alternatively, excessive tissue damage may occur, again compromising survival.
Acute inflammation
Occurs when immune cells resident in the tissue activate upon receiving the stimuli. This happens using the immune cells’ pattern-recognition receptors which recognise either pathogen-associated molecular patterns or damage-associated molecular patterns – molecules either not recognised as belonging to one’s self, or ones recognised as self but exposed only through injury or cell damage. Upon signalling by these receptors, the cells are activated and release inflammatory mediators.
These mediators include signalling molecules called cytokines which attract other immune cells; and vasoactive compounds such as histamine and nitric oxide (NO) which cause blood vessels to dilate and become permeable, thereby allowing blood plasma containing additional immune cells into the tissue at the site of stimulation.
In the plasma are enzymes and antibodies which can immediately attack invading microorganisms, either breaking them open or making them targets (opsonising) for engulfment (phagocytosis) by a kind of immune cells called phagocytes. If the initial response was a wound, then clotting factors will be activated and build the scaffolds required for the repair process.
The recruited immune cells all have specific jobs to do, based on their lineage, location and function. Basophils are the rarest of the white blood cells. Their role is in antigen response, by secreting histamine to dilate blood vessels and heparin to reduce blood clotting and attract neutrophils and eosinophils to the location. These secretory factors are stored within intracellular compartments called granules, and the release of these compounds is called degranulation.
Neutrophils are the most abundant type in blood, comprising up to 70% of total white blood cells. Their role is to respond to bacterial or fungal infection, by engulfing these invaders and destroying them within their intracellular compartments called lysosomes. Their lifespan is limited, especially once their lysosomes are “full”. These cells form the pus at the site of an infection. Eosinophils are less common in blood (only up to 4% of white blood cells), but abundant in mucus membranes such as respiratory, digestive and urinary tracts. These cells respond to parasitic infection, by secreting enzymes to kill parasites that are too big for neutrophils or monocytes to phagocytose.
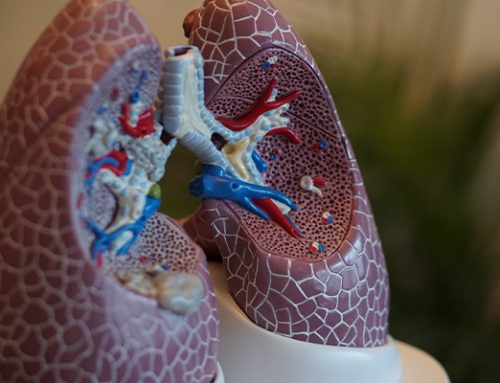
Monocytes are the largest white blood cells. Like neutrophils, their role is to engulf and destroy invaders, but they have a longer lifespan due to their ability to renew their lysosomal contents, and for their other role: they display pieces of invaders on their cell surface for the adaptive immune response. For this reason, they are also known as antigen-presenting cells (APCs). These APCs may also take up residence in fixed locations in the body, where in tissue they are known as macrophages, in the lungs they are known as alvaeolar macrophages, whereas behind the gut wall they are known as dendritic cells; or in the brain they are known as microglia.
APCs secrete cytokines to regulate the local immune environment. APCs are not round like other blood cells but change shape and extend tendrils to move in amoeboid-like fashion and reach between other cells. Macrophages specialise in phagocytosis: they kill their targets with bursts of chemical free radicals such as NO or reactive oxygen species (ROS), and they also engulf dying cells, dead cells and cellular fragments. Dying and dead neutrophils are engulfed by macrophages.
Finally, there are mast cells, a type of connective tissue basophil, very similar in function and appearance, although they are actually a lineage of APC. Mast cells release the same compounds by degranulation as basophils, although triggered by binding of the antibody immunoglobulin E (IgE). Mast cells are involved in defense against invaders, wound healing and immune tolerance – the process of recognising benign non-self stimuli. However, mast cells may become hypersensitive, triggering allergic responses.
Allergies
Are an IgE signalling response which triggers mast cell degranulation. The released histamine is vasodilatory, and triggers nerve endings. This is one of the reasons why allergic responses itch. Mast cell degranulation is involved in asthma, eczema and hayfever (allergic rhinitis). Antihistamines intended to treat this block histamine from triggering nerve endings. Anaphylaxis is a body-wide allergic degranulation of mast cells which causes so much vasodilation that it causes life-threatening shock symptoms.
Chronic inflammation
Occurs when the normal acute response does not end. Normally, once a stimulus is dealt with and any damage is healed then the process of inflammation is resolved. For especially short-lived inflammation then the tissue returns to normal, although if large amounts of tissue destruction occurred during the inflammatory process then fibrous collagen scarring may result. Alternatively, a cavity filled with puss (an abscess) may be left.
However, if the stimulus persists for a long time (such as with autoimmune stimuli (self molecules) or hard-to-remove foreign particles like polluting airborne fine particulate matter less than 2.5 um in diameter known as PM2.5) then the inflammation enters a new phase, dominated by macrophages. These macrophages secrete proinflammatory cytokines to maintain the inflammatory response, and their secretion of NO, ROS, peroxides and protein-degrading enzymes called proteases causes additional destruction and injury and tissue scarring.
Uncontrolled asthma is characterised as chronic inflammation, as are the consequences of long term exposure to PM2.5 air pollution, which can penetrate deep into the lungs and enter the blood stream, thereby distributing to the rest of the body, where it may lodge in other tissues.
Rheumatoid arthritis is another form of chronic allergic inflammation, where a response is mounted against the synovial membranes which encapsulate skeletal joints, ultimately leading to swelling, stiffening, cartilage damage and ultimately bone damage and joint deformation.